Introduction
Overview of Urinary Tract Infections (UTIs)
Urinary Tract Infections (UTIs) are a prevalent health concern, particularly affecting women. These infections occur when bacteria enter the urinary system, which includes the kidneys, ureters, bladder, and urethra. While UTIs can impact anyone, women are significantly more prone due to anatomical and physiological factors. The infection can range from mild to severe, affecting various parts of the urinary tract. Understanding UTIs involves recognizing their symptoms, causes, and the impact they can have on overall health.
Importance of Understanding UTIs
Grasping the nuances of UTIs is crucial for several reasons. First, UTIs are among the most common bacterial infections, with millions of cases reported annually. Awareness can lead to better prevention and management, reducing the risk of recurrent infections and complications. Second, understanding the causes and symptoms helps individuals seek timely medical attention, preventing the infection from escalating into more severe conditions such as kidney infections or sepsis. Finally, dispelling myths and educating about proper hygiene and lifestyle choices can empower individuals to maintain urinary health and improve their quality of life.
What is a Urinary Tract Infection?
Definition and Types of UTIs
A Urinary Tract Infection (UTI) is an infection that affects any part of the urinary system, which includes the kidneys, ureters, bladder, and urethra. UTIs occur when bacteria, typically from the gastrointestinal tract, enter the urinary tract and multiply. The infection can be localized to a specific part of the tract or may involve multiple areas.
There are several types of UTIs based on their location within the urinary system:
- Cystitis: This is an infection of the bladder and is the most common type of UTI. Symptoms often include frequent, painful urination and lower abdominal discomfort.
- Urethritis: This infection affects the urethra, the tube through which urine exits the body. It typically presents with burning sensations during urination and discharge.
- Pyelonephritis: This is a more severe infection that affects one or both kidneys. It can cause flank pain, high fever, and nausea, and often requires more intensive treatment.
- Ureteritis: Although less common, this infection of the ureters (the tubes that carry urine from the kidneys to the bladder) can occur and may be associated with more complex cases of UTI.
Anatomy of the Urinary Tract
Understanding the anatomy of the urinary tract is essential to grasp how UTIs occur and spread. The urinary tract is a complex system designed to produce, store, and eliminate urine, and comprises the following components:
- Kidneys: These are two bean-shaped organs located on either side of the spine. They filter blood to remove waste products and excess fluids, which are then turned into urine.
- Ureters: These are two thin tubes that transport urine from the kidneys to the bladder. They are equipped with muscular walls that propel urine through peristalsis.
- Bladder: The bladder is a hollow, muscular organ that stores urine until it is ready to be expelled from the body. It expands as it fills and contracts during urination.
- Urethra: This is the tube that carries urine from the bladder out of the body. In women, it is shorter, which can make it easier for bacteria to reach the bladder.
Infections typically start in the urethra and can ascend to the bladder and, less commonly, the kidneys. Each part of the urinary tract plays a specific role in the infection's development and symptoms. Understanding this anatomy helps in recognizing how UTIs can impact different parts of the urinary system and informs appropriate treatment and prevention strategies.
Causes of UTIs in Women
Bacterial Infections
The majority of urinary tract infections (UTIs) in women are caused by bacteria. These bacteria can invade the urinary tract and multiply, leading to infection. The most common route of infection is through the urethra, which is relatively short in women, allowing bacteria to travel more easily from the external environment to the bladder.
Bacteria that cause UTIs are often part of the normal flora of the gastrointestinal tract but can become pathogenic under certain conditions. The introduction of these bacteria into the urinary tract can occur through various means, including poor hygiene, sexual activity, or other factors that disrupt the natural barriers that normally prevent bacterial colonization.
Common Bacteria Responsible for UTIs
Other Pathogens
While bacteria are the primary cause of UTIs, other pathogens can also contribute to urinary tract infections. These include:
Understanding the causes of UTIs in women involves recognizing the role of bacterial infections and identifying the specific pathogens responsible. Escherichia coli is the most common culprit, but other bacteria and pathogens can also play a role in urinary tract infections. Awareness of these causes can aid in prevention strategies and guide appropriate treatment, reducing the risk of recurrent or severe infections.
Risk Factors for Women
Urinary Tract Infections (UTIs) are particularly prevalent among women due to a combination of anatomical, hormonal, and lifestyle factors. Understanding these risk factors can help in both prevention and management of UTIs. Here’s a detailed look at the primary risk factors for women:
Anatomical Factors
One of the most significant risk factors for UTIs in women is their anatomical structure. The female urethra is shorter than that of men, measuring approximately 1.5 to 2 inches in length compared to about 8 inches in men. This shorter length allows bacteria easier access to the bladder. Additionally, the proximity of the urethra to the anus increases the risk of bacteria from the gastrointestinal tract entering the urinary tract. Women with anatomical abnormalities, such as a prolapsed bladder or urinary tract anomalies, may also be at higher risk.
Hormonal Changes
Hormonal fluctuations play a crucial role in influencing UTI risk. Estrogen, a key hormone in women, helps maintain the health of the vaginal and urethral mucosa. During hormonal changes, such as those occurring during menopause or pregnancy, estrogen levels can drop, leading to thinning and drying of these tissues. This decreased hormonal support can compromise the natural barriers against bacterial invasion, increasing susceptibility to UTIs. Hormonal contraceptives and hormonal therapies can also impact UTI risk by affecting vaginal flora and pH balance.
Sexual Activity
Sexual activity is a well-established risk factor for UTIs in women. During intercourse, bacteria from the vaginal area or external genitalia can be pushed into the urethra. This is often exacerbated by factors such as frequent sexual activity, use of spermicides, or certain sexual practices. To minimize the risk, it is advised to urinate before and after sexual activity, maintain good genital hygiene, and stay hydrated to help flush out bacteria.
Personal Hygiene Practices
Personal hygiene practices can significantly impact the risk of UTIs. Improper wiping techniques, such as wiping from back to front after using the toilet, can transfer bacteria from the anal region to the urethra. Additionally, the use of irritating feminine hygiene products, such as douches or scented sprays, can disrupt the natural balance of bacteria and yeast in the vaginal area, increasing the risk of infection. Wearing tight-fitting clothing or non-breathable fabrics can also create a warm, moist environment conducive to bacterial growth.
Menopause and Aging
Menopause and aging are critical factors that influence UTI risk in women. As women age, the decline in estrogen levels during menopause leads to changes in the vaginal flora and mucosa. This results in a decrease in protective lactobacilli, which normally help prevent bacterial overgrowth. Postmenopausal women also experience a reduction in vaginal lubrication, which can further increase the likelihood of infections. Aging also impacts immune function and bladder control, making older women more susceptible to UTIs.
Use of Certain Birth Control Methods
Certain birth control methods can also contribute to UTI risk. Spermicides, commonly found in contraceptive products, can disrupt the natural vaginal flora and increase susceptibility to bacterial infections. Diaphragms and condoms with spermicidal lubricants can also irritate the vaginal lining and create a favorable environment for bacteria. Women who use these methods should be aware of their potential impact on urinary health and consider alternative contraceptive options if they experience recurrent UTIs.
Understanding the risk factors for UTIs in women is essential for effective prevention and management. Anatomical factors, hormonal changes, sexual activity, personal hygiene practices, aging, and certain birth control methods all play significant roles in increasing susceptibility to these infections. By addressing these risk factors through preventive measures and lifestyle adjustments, women can reduce their likelihood of developing UTIs and maintain better urinary health.
How Bacteria Enter the Urinary Tract
Understanding how bacteria enter the urinary tract is crucial for grasping the full picture of Urinary Tract Infections (UTIs). This knowledge helps in both prevention and treatment. Here’s an in-depth look at the mechanisms of infection and the common entry points for bacteria.
Mechanisms of Infection
The urinary tract is generally a sterile environment, but it is vulnerable to infection due to its anatomical structure and the presence of bacteria in the surrounding areas. Several mechanisms facilitate bacterial entry and infection:
- Direct Entry: Most UTIs are caused by bacteria that ascend from the urethra to the bladder. Due to the shorter length of the female urethra, bacteria have a shorter distance to travel to reach the bladder. The bacteria can adhere to the urethral lining and multiply, leading to infection.
- Adhesion and Colonization: Bacteria like E. coli possess fimbriae (tiny hair-like projections) that enable them to adhere to the epithelial cells lining the urinary tract. This adhesion is crucial for their survival and multiplication, as it helps them resist being flushed out by urine flow.
- Systemic Infection: Although less common, bacteria can enter the urinary tract through the bloodstream. In cases of systemic infections or sepsis, pathogens from other body parts can be carried to the urinary tract via the bloodstream. This mechanism is more likely in individuals with compromised immune systems or severe infections.
- Regional Infection: Bacteria can also spread to the urinary tract from adjacent infected tissues via the lymphatic system. This route is rare but can occur in cases of pelvic infections or tumors that invade or affect the lymph nodes connected to the urinary tract.
Common Entry Points for Bacteria
Several entry points facilitate the introduction of bacteria into the urinary tract. Understanding these points helps in identifying risk factors and implementing preventive measures:
- External Environment: The urethra is the most common entry point for bacteria. Bacteria from the perineum or genital area can easily enter the urethra, especially if hygiene practices are inadequate. Factors such as improper wiping techniques (wiping from back to front) can transfer bacteria from the anal area to the urethra.
- Sexual Activity: During sexual intercourse, bacteria can be pushed into the urethra from the genital area or partner. This is why women are advised to urinate after sex to help flush out any bacteria that may have entered the urethra.
- Indwelling Catheters: Urinary catheters, which are used to manage urinary retention or in hospital settings, can serve as a conduit for bacteria to enter the urinary tract. The insertion and maintenance of catheters can introduce bacteria directly into the bladder. Proper catheter care and hygiene are essential to prevent catheter-associated UTIs.
- Bacterial Overgrowth: The vaginal flora, which includes various bacteria and yeasts, can sometimes become imbalanced. An overgrowth of harmful bacteria or yeast can lead to infections that migrate to the urinary tract. Hormonal changes, antibiotics, or changes in personal hygiene practices can affect the balance of vaginal flora.
- Postpartum Period: Women who have recently given birth are at a higher risk of UTIs due to potential changes in vaginal flora and increased exposure to bacteria during labor and delivery. Postpartum women may need to take extra precautions with personal hygiene to reduce the risk of infection.
- Chronic Health Issues: Conditions like diabetes or immunocompromised states can affect the body’s ability to ward off infections. High blood sugar levels in diabetes can promote bacterial growth, making it easier for bacteria to invade the urinary tract.
Bacteria can enter the urinary tract through various mechanisms and entry points, with the urethra being the most common route. Understanding how bacteria reach the urinary tract helps in devising effective prevention strategies and treatment plans. By addressing the risk factors associated with bacterial entry and maintaining good hygiene practices, individuals can significantly reduce their risk of developing UTIs and promote overall urinary health.
Symptoms of a UTI
Urinary Tract Infections (UTIs) can present with a range of symptoms, from mild discomfort to severe, alarming signs. Recognizing these symptoms is crucial for timely treatment and preventing complications. Here’s a detailed overview of both common and severe symptoms associated with UTIs:
Common Symptoms
Severe Symptoms Requiring Immediate Attention
Recognizing the symptoms of a UTI is essential for effective management and treatment. While common symptoms such as frequent urination and burning sensations are indicative of a UTI, severe symptoms like high fever, flank pain, and blood in urine signal more serious conditions that require immediate medical attention. Timely intervention can prevent complications and ensure effective treatment, promoting better urinary health and overall well-being.
Diagnosis of UTIs
Diagnosing a Urinary Tract Infection (UTI) involves a combination of evaluating symptoms, performing laboratory tests, and sometimes using imaging techniques. Accurate diagnosis is essential for effective treatment and management. Here’s a comprehensive overview of the diagnostic process for UTIs:
Medical History and Symptom Review
- Patient History: The healthcare provider will begin by taking a detailed medical history. This includes asking about previous UTIs, any underlying health conditions (e.g., diabetes, kidney disease), and any current medications. The history of urinary symptoms and previous episodes of UTIs can provide crucial insights.
- Sexual and Gynecological History: For women, the provider may inquire about sexual activity, contraceptive use, and menstrual history. These factors can influence the risk of UTIs and are important for a comprehensive evaluation.
- Symptom Description: The healthcare provider will ask about the specific symptoms experienced, including frequency of urination, pain or burning sensations, presence of blood in the urine, and any abdominal or back pain. The pattern and severity of symptoms help guide further testing and diagnosis.
- Onset and Duration: Information about when the symptoms started and their duration helps determine whether the infection is acute or chronic, which can influence treatment decisions.
Urinalysis and Urine Culture
- Initial Screening: Urinalysis is a common initial test used to detect signs of infection. A urine sample is examined for the presence of:
- White Blood Cells (WBCs): Elevated levels indicate an inflammatory response to infection.
- Red Blood Cells (RBCs): The presence of blood may suggest a more severe infection or other urinary tract issues.
- Nitrites: Many bacteria produce nitrites, which can be detected in the urine and suggest a bacterial infection.
- Leukocyte Esterase: This enzyme, produced by white blood cells, can indicate an infection.
- Protein and Glucose: Abnormal levels may indicate other conditions affecting the kidneys or diabetes.
- Confirmatory Test: A urine culture is used to identify the specific bacteria causing the infection. A sample of urine is cultured in a lab to allow bacteria to grow, which helps determine the exact pathogen.
- Antibiotic Sensitivity Testing: Once bacteria are identified, sensitivity testing is conducted to determine which antibiotics are most effective against the specific strain. This helps in selecting the appropriate treatment and avoiding antibiotic resistance.
Imaging Tests
- Assessment of Urinary Tract: An ultrasound of the kidneys and bladder can help visualize any abnormalities, such as kidney stones, tumors, or structural anomalies that may be contributing to the infection or symptoms.
- Detailed Imaging: A computed tomography (CT) scan may be used for a more detailed view of the urinary tract, especially if there are complications or if the initial tests are inconclusive. A CT scan can help identify kidney stones, abscesses, or other issues that may complicate a UTI.
- Less Common: Magnetic Resonance Imaging (MRI) is less frequently used but may be indicated in complex cases where detailed imaging is required, particularly if there is suspicion of malignancy or if the patient cannot undergo a CT scan due to allergies or other factors.
The diagnosis of a UTI involves a thorough review of medical history and symptoms, followed by diagnostic tests such as urinalysis and urine culture. Imaging tests may be employed if there are complications or if initial tests are inconclusive. Accurate diagnosis is essential for effective treatment and to address any underlying issues that may contribute to urinary tract infections. By following a structured diagnostic approach, healthcare providers can ensure appropriate management and help prevent recurrent infections.
Prevention Strategies for UTIs
Preventing Urinary Tract Infections (UTIs) involves adopting several strategies to reduce the risk of bacterial invasion and infection. By incorporating proper hygiene practices, maintaining good hydration, and taking other preventive measures, individuals can significantly lower their chances of developing UTIs. Here’s a detailed look at effective prevention strategies:
Proper Hygiene Practices
- Front to Back: Always wipe from front to back after using the toilet. This practice helps prevent the transfer of bacteria from the anal area to the urethra, reducing the risk of infection.
- Personal Care Products: Use mild, unscented soaps and avoid douches, sprays, or other feminine hygiene products that can disrupt the natural balance of bacteria and yeast in the vaginal area.
- Breathable Fabrics: Wear cotton underwear and avoid tight-fitting clothing. Breathable fabrics help keep the genital area dry and reduce the risk of bacterial growth.
- Genital Hygiene: Maintain regular hygiene of the genital area, but avoid over-washing or using harsh soaps that can lead to irritation or imbalance.
Hydration and Diet Tips
- Increase Fluid Intake: Drink plenty of water throughout the day. Staying well-hydrated helps flush out bacteria from the urinary tract and reduces the risk of infection. Aim for at least 8 glasses of water daily, or more if you are active or live in a hot climate.
- Potential Benefits: Some studies suggest that cranberry juice or supplements may help prevent UTIs by inhibiting bacteria from adhering to the urinary tract. While not a cure, incorporating cranberry products into your diet may provide additional protection.
- Nutritional Support: Eat a balanced diet rich in fruits, vegetables, and whole grains. A healthy diet supports overall immune function and can help your body resist infections.
Post-Sexual Activity Care
- Flush Out Bacteria: Urinate shortly after sexual activity to help flush out any bacteria that may have entered the urethra during intercourse. This simple step can significantly reduce the risk of developing a UTI.
- Cleanliness: Wash the genital area with water after sexual activity to remove any bacteria. Avoid using harsh soaps or douches that may disrupt the natural flora.
Regular Medical Check-ups
- Monitoring Health: Regular check-ups with a healthcare provider can help monitor and manage any chronic conditions that may increase the risk of UTIs. This includes managing diabetes, kidney health, and other related issues.
- Professional Evaluation: If you experience recurrent UTIs, consult with your healthcare provider for a thorough evaluation. They may conduct tests to identify underlying issues or recommend preventive strategies, such as long-term low-dose antibiotics or other treatments.
- Adherence to Treatment: If diagnosed with a UTI, follow your healthcare provider’s recommendations for treatment and follow-up care. Completing the full course of prescribed antibiotics is crucial for fully eradicating the infection and preventing recurrence.
Implementing prevention strategies for UTIs involves a multifaceted approach that includes maintaining proper hygiene, staying hydrated, practicing good post-sexual activity care, and engaging in regular medical check-ups. By adopting these preventive measures, individuals can significantly reduce their risk of developing UTIs and maintain better urinary health.
Treatment Options for UTIs
Effectively treating a Urinary Tract Infection (UTI) involves a combination of prescribed medications, home remedies, and lifestyle adjustments. Knowing when to seek medical attention is also crucial for managing the infection and preventing complications. Here’s a detailed overview of treatment options:
Antibiotic Medications
- First-Line Treatment: Antibiotics are the primary treatment for UTIs and are prescribed based on the type of bacteria causing the infection. Commonly prescribed antibiotics include trimethoprim-sulfamethoxazole, nitrofurantoin, ciprofloxacin, and amoxicillin.
- Duration and Dosage: The duration of antibiotic treatment typically ranges from 3 to 7 days, depending on the severity and location of the infection. It’s essential to complete the full course of antibiotics, even if symptoms improve, to ensure the infection is fully eradicated and to prevent antibiotic resistance.
- Customized Treatment: In some cases, a urine culture may be performed to identify the specific bacteria and determine the most effective antibiotic. This helps in targeting the infection more accurately and avoiding unnecessary antibiotic use.
Home Remedies and Lifestyle Changes
- Hydration: Drinking plenty of water helps flush out bacteria from the urinary tract. Aim for at least 8 glasses of water per day to support the body's natural cleansing processes.
- Potential Benefits: While not a substitute for antibiotics, cranberry juice or supplements may help prevent bacteria from adhering to the urinary tract. It can be a useful adjunctive measure for those prone to recurrent UTIs.
- Pain Relief: Applying a heating pad or warm compress to the lower abdomen can help relieve discomfort and reduce cramping associated with UTIs.
- Personal Care Products: Refrain from using irritating feminine hygiene products, such as douches or scented sprays, that can disrupt the natural balance of the urinary tract and exacerbate symptoms.
When to See a Doctor
- Professional Evaluation: If symptoms persist despite home remedies or worsen over time, consult a healthcare provider. Persistent symptoms may indicate a more severe infection or complications.
- Underlying Issues: Frequent or recurrent UTIs warrant a thorough medical evaluation to identify and address any underlying conditions or anatomical abnormalities that may be contributing to the infections.
- Seek Immediate Care: If you experience high fever, severe flank pain, nausea, vomiting, or signs of confusion, seek immediate medical attention. These symptoms could indicate a more serious infection, such as pyelonephritis, or complications requiring urgent treatment.
- Alternative Management: If symptoms do not improve or if you have concerns about the effectiveness of prescribed antibiotics, consult your doctor. They may need to adjust the treatment plan or conduct further testing to address the issue.
Treating a UTI effectively involves a combination of antibiotics, home remedies, and lifestyle changes. While antibiotics remain the cornerstone of treatment, supportive measures such as increased hydration and heat therapy can provide symptom relief. It’s important to seek medical attention if symptoms are severe, persistent, or recurrent, to ensure proper management and prevent complications. By following these treatment options and guidelines, individuals can effectively manage UTIs and promote better urinary health.
Complications of Untreated UTIs
Untreated Urinary Tract Infections (UTIs) can lead to a range of complications, affecting not only the urinary system but also broader aspects of health. Here’s an overview of the possible health risks and impacts on reproductive health associated with untreated UTIs:
Possible Health Risks
- Infection Spread: If a UTI is left untreated, bacteria can travel from the bladder to the kidneys, leading to a more severe infection known as pyelonephritis. This condition is characterized by high fever, flank pain, nausea, and vomiting.
- Potential Consequences: Pyelonephritis can cause long-term damage to the kidneys, potentially leading to kidney scarring or chronic kidney disease if not addressed promptly.
- Systemic Infection: In severe cases, the bacteria from a UTI can enter the bloodstream, causing sepsis. Sepsis is a life-threatening condition that leads to widespread inflammation, organ failure, and can be fatal if not treated urgently.
- Symptoms: Symptoms of sepsis include extreme fever or chills, rapid heart rate, confusion, and shortness of breath, requiring immediate medical intervention.
- Increased Frequency: Untreated UTIs can lead to recurrent infections, which may become more difficult to treat over time. Repeated infections can cause chronic discomfort and may require more aggressive treatment.
- Chronic Inflammation: Persistent infection can lead to chronic inflammation and damage to the bladder lining. This can result in ongoing symptoms such as pain, urgency, and frequency, even after the infection has been treated.
Impact on Reproductive Health
- Risk to Mother and Baby: UTIs during pregnancy can pose risks to both the mother and the unborn child. Untreated infections can increase the risk of preterm labor, low birth weight, and complications such as preeclampsia.
- Management: Pregnant women should receive prompt treatment for UTIs to minimize these risks and ensure a healthy pregnancy outcome.
- Menstrual Irregularities: Chronic UTIs can sometimes contribute to menstrual irregularities or exacerbate existing gynecological issues. The stress and discomfort associated with ongoing infections can affect menstrual cycles.
- Increased Sensitivity: Persistent UTIs can cause discomfort or pain during sexual activity. The irritation and inflammation in the urinary tract can make sexual intercourse uncomfortable or painful.
- Risk of Transmission: Although UTIs themselves are not sexually transmitted, the presence of an infection can sometimes be exacerbated by sexual activity. Proper post-sexual hygiene can help reduce this risk.
- Spread of Infection: In women, untreated UTIs may sometimes spread to the reproductive organs, leading to pelvic inflammatory disease (PID). PID is an infection of the uterus, fallopian tubes, and ovaries, which can cause chronic pelvic pain and infertility.
Untreated UTIs can lead to significant health risks, including severe kidney infections, sepsis, and chronic bladder damage. The impact on reproductive health can also be substantial, affecting pregnancy outcomes, menstrual health, and sexual well-being. Early detection and treatment of UTIs are crucial to prevent these complications and maintain overall health. If you experience symptoms of a UTI, seek medical advice promptly to avoid these potential risks.
When to Seek Medical Help
Knowing when to seek medical help for a Urinary Tract Infection (UTI) is crucial for preventing complications and ensuring effective treatment. Here’s a guide to recognizing signs of severe infection and understanding when self-treatment might not be sufficient:
Signs of Severe Infection
- Temperature Above 101°F (38.3°C): A high fever, especially when accompanied by chills and sweating, can indicate a more serious infection, such as pyelonephritis (kidney infection) or sepsis. Immediate medical evaluation is needed.
- Intense Pain in the Lower Back: Severe pain on one side of the lower back or abdomen can signal a kidney infection. This type of pain is usually more intense than the discomfort associated with a bladder infection.
- Systemic Symptoms: Persistent nausea and vomiting can be signs that the infection has spread beyond the bladder. These symptoms, combined with fever or flank pain, require urgent medical attention.
- Visible or Microscopic Hematuria: The presence of blood in the urine, whether visible or detected during a urinalysis, may indicate a more severe infection or complications like kidney stones.
- Mental Status Changes: Especially in older adults, confusion, delirium, or disorientation can be symptoms of a severe infection or sepsis. These signs need immediate medical evaluation.
When Self-Treatment is Not Enough
- No Improvement: If symptoms such as burning during urination, frequent urination, or lower abdominal pain persist despite self-care measures like hydration and over-the-counter pain relief, it is essential to seek medical attention.
- Recurrent UTIs: If you experience frequent UTIs, which are infections occurring more than twice a year, or if the infection recurs shortly after treatment, consult a healthcare provider. Persistent or recurrent UTIs may require further investigation and specialized treatment.
- Chronic Health Issues: Individuals with chronic health conditions, such as diabetes or immune system disorders, should seek medical advice if they suspect a UTI. These conditions can complicate infection and require tailored treatment approaches.
- Complicated UTIs: If you develop symptoms indicating possible complications, such as severe pain, high fever, or systemic symptoms like nausea and vomiting, it is crucial to seek prompt medical care. These symptoms may indicate that the infection has spread or led to serious health issues.
- Lack of Improvement: If you have been prescribed antibiotics and symptoms do not improve or worsen, contact your healthcare provider. They may need to adjust the treatment plan or perform additional tests to address the infection effectively.
Prompt medical attention is necessary when experiencing signs of severe infection or if self-treatment measures are insufficient. Recognizing symptoms like high fever, severe pain, or persistent symptoms despite home care is crucial for preventing complications and ensuring effective management of UTIs. Seeking professional medical help allows for appropriate diagnosis and treatment, reducing the risk of serious health issues.
Myths and Misconceptions about UTIs
Understanding the truth about Urinary Tract Infections (UTIs) helps in effective prevention and treatment. Here’s a look at some common myths and misconceptions, along with clarifications to clear up any misunderstandings:
Common Misunderstandings
- Clarification: While poor hygiene can contribute to UTIs, they are not always caused by it. UTIs can result from various factors including anatomical differences, hormonal changes, and even genetic predispositions. Good hygiene is important, but it’s not the sole cause of UTIs.
- Clarification: Although sexual activity can increase the risk of UTIs, it is not the only cause. Bacteria can enter the urinary tract through other means, such as improper wiping, use of certain birth control methods, or even from daily activities that may introduce bacteria.
- Clarification: Cranberry juice may help prevent UTIs by preventing bacteria from adhering to the urinary tract, but it is not a cure. Antibiotics are required to treat an active UTI. Cranberry juice can be a helpful preventive measure but should not replace medical treatment.
- Clarification: UTIs are not STIs, although they can sometimes be confused with symptoms of STIs. UTIs are caused by bacteria that infect the urinary tract, while STIs are transmitted through sexual contact and involve different pathogens.
- Clarification: While women are more prone to UTIs due to anatomical factors, men can also get UTIs. Factors like urinary tract obstructions, catheter use, and certain medical conditions can increase the risk for men.
- Clarification: Drinking plenty of fluids is actually recommended when you have a UTI. Hydration helps flush bacteria from the urinary tract and can aid in reducing symptoms. Avoiding fluids can exacerbate symptoms and delay recovery.
- Clarification: While antibiotics are effective in treating UTIs, it’s important to complete the full course as prescribed. Some UTIs may require longer treatment or different antibiotics, especially if caused by antibiotic-resistant bacteria.
- Clarification: UTIs can lead to serious complications if left untreated, including kidney infections and sepsis. It’s important to address symptoms promptly to prevent these potential complications and ensure appropriate treatment.
Clearing up myths and misconceptions about UTIs helps in better understanding and managing the condition. Recognizing that UTIs can be caused by various factors, not just poor hygiene or sexual activity, and understanding the role of cranberry juice and antibiotics can lead to more effective prevention and treatment strategies. Accurate information is key to managing UTIs effectively and avoiding unnecessary complications.
Shri Chyawan’s Ayurvedic Solution
Urinary Infection: Urinary Infection causes problems in the urinary system such as kidney, and bladder infections. Most of the infections take place in the lower urinary tract. If, these urinary infections whether in men or women are not treated in time, then they might result in kidney damage.
Symptoms of Urinary infection: This mostly depends on which part of the urinary tract has been infected, symptoms of these include:
- Burning/inflammation sensation while urinating
- Frequent urination
- Cloudy urine
- Color change in urine
Shri Chyawan Ayurveda's Urinating Care Kit includes the following:
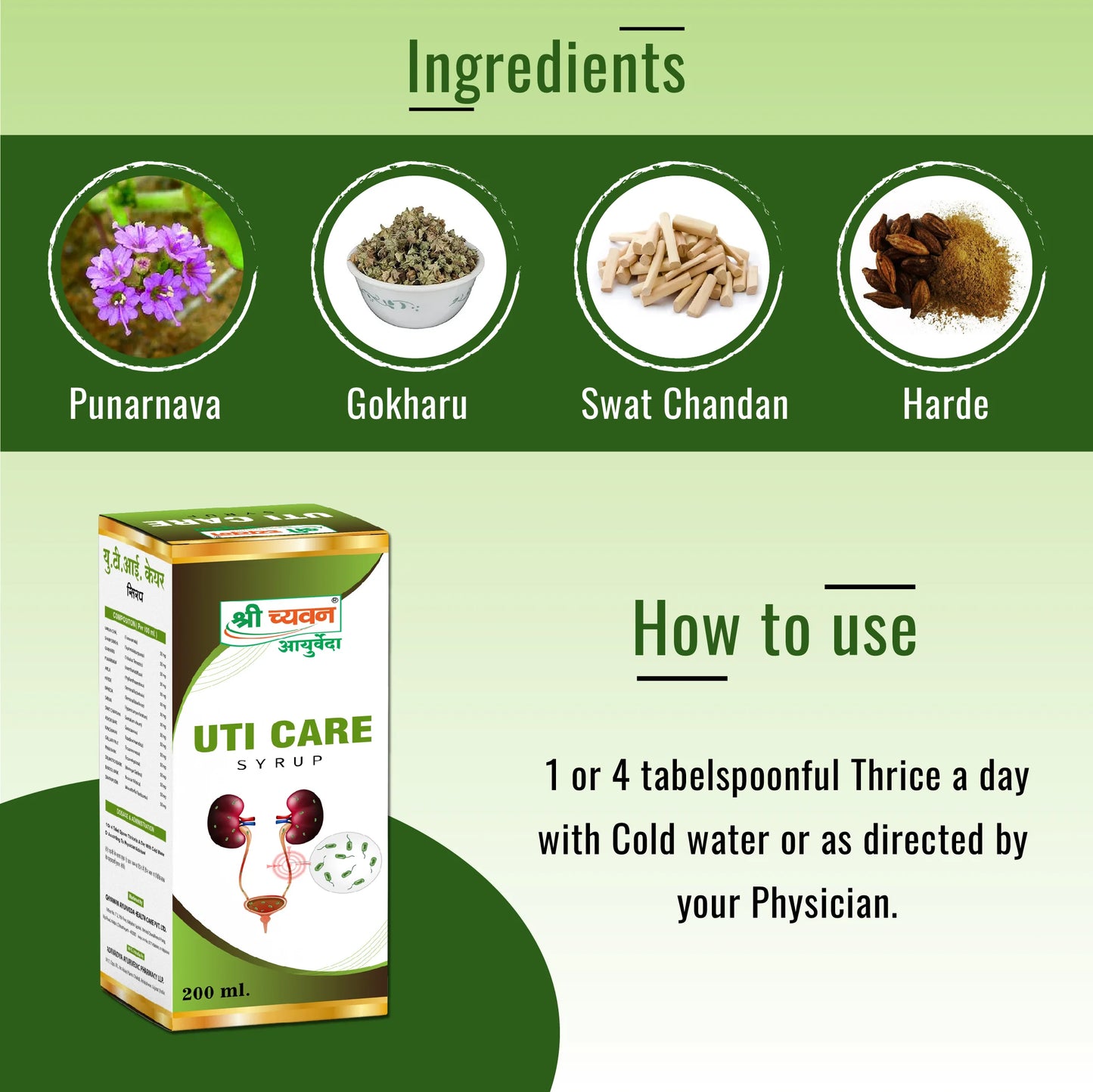
1. Uti Care Syrup: One of the effective ayurvedic syrup for urine infection, useful in curing Urine Infections and Urine blockages. It also acts as a detoxifier for your body and cleanses your system.
Ingredients: It consists of mainly Varun Chal, Sharpunkha, Gokharu, Punarnava, Amle, Harde, Baheda, Sariva, Swat Chandan, Ashok Bark, Kanchanar, Gullar Fruit, Pipar Bark, Drumstick Bark, Babbol Bark, Dhatkipuspa.
How to use: Consume 1 teaspoon thrice a day with cold water or as directed by the physician.
2. Chandraprabha Vati: Chandraprabha Vati helps to reduce the level of uric acid, which aids in keeping urinary infections away.
Ingredients: It consists Swarn Bhasm, Vai Vidang, Chitrak Bark, Daruharidra, Devdaru, Camphor, Pipalmool, Nagarmotha, Pippal, Kali Mirch, Yavkshar, Vach, Dhania, Chavya, Gajpipal, Sounth, Sendha Namak, Nishoth, Dantimool, Tejpatra, Chhoti elaichi.
How To Use: Consume 1 tablet at night before going to bed. consulting a healthcare professional before use.
Conclusion
Understanding and managing Urinary Tract Infections (UTIs) is crucial for maintaining urinary health and overall well-being. Here’s a recap of key points and encouragement for prevention and early treatment:
Recap of Key Points
- UTIs are infections that affect the urinary tract, which includes the bladder, urethra, ureters, and kidneys. They are primarily caused by bacteria, with common culprits being E. coli, but can also involve other pathogens.
- Common symptoms include frequent urination, burning sensation during urination, cloudy or strong-smelling urine, and lower abdominal pain. Severe symptoms may involve high fever, flank pain, nausea, and blood in the urine.
- Factors such as anatomical differences, hormonal changes, sexual activity, poor personal hygiene practices, and certain birth control methods can increase the risk of developing a UTI.
- UTIs are diagnosed through a combination of medical history, urinalysis, urine culture, and, if necessary, imaging tests to identify and address complications.
- The primary treatment for UTIs involves antibiotics prescribed based on the specific bacteria identified. Home remedies and lifestyle changes, such as increased hydration and heat therapy, can support recovery but should not replace medical treatment.
- Untreated UTIs can lead to severe complications, including kidney infections, sepsis, chronic bladder damage, and impacts on reproductive health. Prompt treatment is essential to prevent these risks.
- Effective prevention strategies include maintaining proper hygiene, staying hydrated, practicing good post-sexual activity care, and attending regular medical check-ups. Adopting these habits can significantly reduce the risk of UTIs.
- Common myths include the beliefs that UTIs are only caused by poor hygiene or sexual activity, and that cranberry juice can cure them. Clarifying these misconceptions helps in understanding and managing UTIs more effectively.
Encouragement for Prevention and Early Treatment
Preventing UTIs is often more manageable than treating them after they occur. By adopting good hygiene practices, staying well-hydrated, and following preventive measures, you can significantly lower your risk of developing a UTI. Recognize the signs of a UTI early and seek prompt medical attention to avoid complications and ensure effective treatment.
If you experience symptoms of a UTI, do not hesitate to consult a healthcare provider. Early intervention not only aids in quicker recovery but also helps prevent serious health issues. Embracing these preventive strategies and understanding the nature of UTIs will empower you to take proactive steps towards maintaining optimal urinary health.
By staying informed and vigilant, you can reduce the frequency of UTIs and address them effectively when they arise, leading to better health and well-being.
FAQs: Commonly Asked Questions About UTIs
-
What is a UTI?
- Answer: A Urinary Tract Infection (UTI) is an infection that affects any part of the urinary system, including the bladder, urethra, ureters, and kidneys. It is most commonly caused by bacteria, primarily Escherichia coli (E. coli), but can involve other pathogens.
- What are the typical symptoms of a UTI?
- Answer: Common symptoms include frequent and urgent need to urinate, a burning sensation during urination, cloudy or strong-smelling urine, lower abdominal pain, and sometimes blood in the urine. Severe symptoms may involve high fever, chills, nausea, and vomiting.
- How can I prevent UTIs?
- Answer: Preventive measures include drinking plenty of water, practicing proper hygiene (wiping front to back), urinating after sexual activity, avoiding irritants like douches, and maintaining a healthy diet. For women, wearing breathable cotton underwear and avoiding tight clothing can also help.
- Are UTIs more common in women than in men?
- Answer: Yes, UTIs are more common in women due to anatomical differences; women have a shorter urethra, which makes it easier for bacteria to reach the bladder. However, men can also get UTIs, especially if they have conditions that affect the urinary tract.
- Can UTIs be treated with home remedies?
- Answer: While home remedies such as drinking cranberry juice, increasing fluid intake, and using heat therapy can support UTI management and symptom relief, they should not replace medical treatment. Antibiotics prescribed by a healthcare provider are necessary to fully treat a UTI.
- How long does it take for antibiotics to work?
- Answer: Antibiotics usually start relieving symptoms within a few days, but it’s important to complete the full course as prescribed, even if you feel better. This ensures the infection is fully cleared and helps prevent antibiotic resistance.
- When should I see a doctor for a UTI?
- Answer: Seek medical attention if you experience severe symptoms, such as high fever, severe pain, nausea, or blood in the urine. Also, consult a doctor if symptoms persist despite home treatment, if you have frequent UTIs, or if you have underlying health conditions that could complicate the infection.
- Can UTIs lead to serious health problems if untreated?
- Answer: Yes, untreated UTIs can lead to serious complications such as kidney infections (pyelonephritis), sepsis, and chronic bladder damage. Prompt treatment is essential to prevent these risks and ensure proper recovery.
- Is it safe to have sexual activity with a UTI?
- Answer: It’s generally advised to avoid sexual activity while experiencing UTI symptoms to prevent worsening the infection. If you have frequent UTIs related to sexual activity, discuss preventive strategies with your healthcare provider.
- Can UTIs affect pregnancy?
- Answer: Yes, UTIs can affect pregnancy by increasing the risk of complications such as preterm labor, low birth weight, and preeclampsia. Pregnant women should receive prompt treatment for UTIs to minimize these risks and ensure a healthy pregnancy.
- Are there any long-term effects of recurrent UTIs?
- Answer: Recurrent UTIs can lead to chronic urinary issues, bladder damage, or kidney problems if not managed effectively. Regular check-ups and preventive measures are important to address the underlying causes and reduce recurrence.
- How can I distinguish between a UTI and other conditions with similar symptoms?
- Answer: Symptoms of a UTI can overlap with other conditions like sexually transmitted infections (STIs) or bladder conditions. A healthcare provider can perform diagnostic tests such as urinalysis and urine culture to accurately identify a UTI and differentiate it from other conditions.
Free Consultation with our Expert Doctor- 📞📞 95162 64444