Introduction
Urinary Tract Infections (UTIs) are a common and often troubling health issue that can significantly impact quality of life. For many individuals, the experience of UTIs is not limited to a single episode but rather becomes a recurring problem. Frequent UTIs can lead to frustration, discomfort, and a range of complications if not managed effectively. Understanding why UTIs keep coming back is crucial for developing effective strategies to prevent and treat these infections.
Overview of Frequent UTIs
A Urinary Tract Infection (UTI) occurs when bacteria enter and multiply in the urinary tract, causing inflammation and infection. While a single UTI is uncomfortable enough, frequent UTIs are those that recur several times a year or more. This persistent issue can affect any part of the urinary tract, including the urethra, bladder, ureters, and kidneys.
Key Characteristics of Frequent UTIs:
- Recurring Symptoms: Individuals with frequent UTIs experience symptoms such as burning during urination, frequent urges to urinate, and lower abdominal discomfort on a recurring basis.
- Chronic Infections: In some cases, UTIs can become chronic, with symptoms lingering despite treatment or returning soon after the completion of antibiotic therapy.
- Impact on Quality of Life: Frequent UTIs can significantly disrupt daily activities, cause emotional distress, and lead to complications if not effectively managed.
Understanding why UTIs recur frequently involves examining a variety of factors, including anatomical, physiological, and lifestyle elements. Identifying these underlying causes is essential for effective treatment and prevention.
Importance of Understanding Recurrence
- Improving Treatment Outcomes:
Understanding the reasons behind recurrent UTIs allows for more targeted and effective treatment. If the underlying cause of frequent infections is not addressed, treatment may only offer temporary relief. For instance:
- Antibiotic Resistance: Identifying whether bacteria are resistant to commonly prescribed antibiotics helps in choosing the right medication and preventing ineffective treatments.
- Chronic Conditions: Recognizing chronic medical conditions or anatomical abnormalities that contribute to recurrent UTIs enables tailored treatments and preventive measures.
- Preventing Complications:
Frequent UTIs can lead to serious complications if not properly managed:
- Kidney Damage: Persistent infections, particularly those affecting the upper urinary tract, can lead to kidney damage and long-term health issues.
- Sepsis: In severe cases, recurrent UTIs can escalate to sepsis, a potentially life-threatening condition that requires immediate medical attention.
- Enhancing Quality of Life:
Frequent UTIs can have a profound impact on an individual’s quality of life, causing discomfort and interfering with daily activities. By understanding and addressing the causes of recurrence, individuals can achieve better management of their condition, reduce the frequency of infections, and improve their overall well-being.
- Guiding Preventive Measures:
Knowledge of the factors contributing to recurrent UTIs helps in implementing effective preventive strategies. This may include:
- Lifestyle Adjustments: Changes in personal hygiene, diet, and fluid intake can significantly impact UTI recurrence.
- Medical Interventions: Prophylactic antibiotics or other treatments may be recommended based on the underlying causes of frequent infections.
- Reducing Healthcare Costs:
Addressing recurrent UTIs effectively can help reduce the need for repeated medical visits, tests, and treatments. This not only benefits the individual by minimizing disruption but also reduces overall healthcare costs associated with managing frequent infections.
In summary, understanding the reasons behind frequent UTIs is crucial for improving treatment, preventing complications, enhancing quality of life, and implementing effective preventive measures. By exploring the factors that contribute to recurrent infections, individuals and healthcare providers can work together to manage and reduce the impact of UTIs.
Understanding Urinary Tract Infections
Urinary Tract Infections (UTIs) are a widespread health concern that can affect individuals of all ages and backgrounds. They occur when bacteria enter and infect any part of the urinary system. Understanding what a UTI is, the common causes behind these infections, and how they affect the body can help in managing and preventing them effectively.
What is a UTI?
A Urinary Tract Infection (UTI) is an infection that occurs in any part of the urinary system, which includes:
- Urethra: The tube through which urine exits the body.
- Bladder: The organ that stores urine.
- Ureters: The tubes that carry urine from the kidneys to the bladder.
- Kidneys: The organs that filter blood to produce urine.
UTIs are primarily caused by bacteria, though fungi and viruses can also be responsible in rare cases. The most common bacteria causing UTIs is Escherichia coli (E. coli), which is normally found in the intestines but can invade the urinary tract.
Types of UTIs:
- Cystitis: Infection of the bladder. This is the most common type of UTI and usually results in symptoms like frequent, painful urination and lower abdominal discomfort.
- Urethritis: Infection of the urethra. It often presents with symptoms such as burning sensation during urination and discharge.
- Pyelonephritis: Infection of the kidneys. This type is more serious and can cause symptoms such as fever, chills, and flank pain, and may lead to more severe complications if left untreated.
- Acute Prostatitis: Inflammation of the prostate gland in men, which can be caused by a UTI.
Common Causes of UTIs
UTIs are generally caused by bacteria entering the urinary tract. Several factors can contribute to the development of UTIs:
- Bacterial Entry:
- E. coli: The majority of UTIs are caused by E. coli, which is normally present in the intestines. These bacteria can travel from the anus to the urethra and ascend to the bladder.
- Other Bacteria: Less commonly, UTIs can be caused by other bacteria, including Klebsiella, Proteus, Enterococcus, and Pseudomonas.
- Anatomical Factors:
- Short Urethra in Women: Women have a shorter urethra than men, which makes it easier for bacteria to reach the bladder.
- Enlarged Prostate in Men: An enlarged prostate can obstruct urine flow and increase the risk of infection.
- Sexual Activity:
- Post-Coital UTIs: Sexual activity can introduce bacteria into the urethra. Women who are sexually active may be at higher risk, especially if they do not urinate after intercourse.
- Personal Hygiene Practices:
- Improper Wiping: Wiping from back to front can transfer bacteria from the anus to the urethra.
- Use of Irritants: Certain hygiene products, such as douches or sprays, can irritate the urethra and increase infection risk.
- Urinary Tract Abnormalities:
- Structural Abnormalities: Congenital or acquired abnormalities in the urinary tract can lead to incomplete bladder emptying or reflux, increasing the risk of infection.
- Kidney Stones: Stones can obstruct urine flow and provide a surface for bacterial growth.
- Medical Conditions:
- Diabetes: High blood sugar levels can impair the immune system and provide a nutrient-rich environment for bacteria.
- Immunocompromised Conditions: Conditions that weaken the immune system, such as HIV or cancer treatments, can increase susceptibility to infections.
- Indwelling Catheters:
- Urinary Catheters: Long-term use of urinary catheters can introduce bacteria into the bladder and lead to infections.
How UTIs Affect the Body
When bacteria infect the urinary tract, they cause inflammation and disrupt normal urinary function. The effects on the body depend on the location and severity of the infection:
- Bladder (Cystitis):
- Symptoms: Painful urination, frequent urination, urgency, lower abdominal pain, and sometimes blood in the urine.
- Impact: Inflammation of the bladder lining causes discomfort and can affect the bladder’s ability to store urine efficiently.
- Urethra (Urethritis):
- Symptoms: Burning sensation during urination, discharge, and discomfort in the urethra.
- Impact: Inflammation of the urethra can cause pain and difficulty with urination.
- Kidneys (Pyelonephritis):
- Symptoms: Fever, chills, flank pain (pain in the side or back), nausea, and vomiting. In severe cases, symptoms may include confusion and rapid heartbeat.
- Impact: Infection of the kidneys can lead to more serious complications, including kidney damage and sepsis if not treated promptly.
- Overall Impact:
- Systemic Effects: If UTIs are severe or untreated, the infection can spread to the bloodstream, leading to sepsis, a life-threatening condition characterized by widespread inflammation and organ dysfunction.
- Chronic Symptoms: Recurrent UTIs can lead to chronic discomfort, emotional stress, and complications such as kidney damage or scarring.
Understanding UTIs, their causes, and their effects on the body helps in recognizing symptoms early, seeking appropriate treatment, and implementing preventive measures to reduce the risk of recurrence.
Factors Contributing to Frequent UTIs
Frequent Urinary Tract Infections (UTIs) can be attributed to a variety of factors ranging from anatomical and hormonal changes to lifestyle practices and chronic medical conditions. Understanding these factors is crucial for effectively managing and preventing recurrent UTIs. Below is a detailed exploration of the primary contributors to frequent UTIs.
Anatomical Factors
Female Anatomy and UTIs:
- Shorter Urethra: Women have a shorter urethra compared to men, which means bacteria have a shorter distance to travel to reach the bladder. This anatomical feature increases the likelihood of UTIs.
- Proximity to the Anus: The female urethra is close to the anus, which can facilitate the transfer of bacteria from the rectal area to the urinary tract, especially if proper hygiene is not maintained.
- Vaginal Flora: The presence of certain bacteria in the vaginal area can influence UTI risk. Disruptions in the balance of vaginal flora, such as those caused by antibiotics or hormonal changes, can increase susceptibility.
Male Anatomy and UTIs:
- Longer Urethra: Men have a longer urethra, which provides a greater distance for bacteria to travel before reaching the bladder. This generally reduces the risk of UTIs in men compared to women.
- Prostate Issues: An enlarged prostate or prostatitis can obstruct urine flow and increase the risk of UTIs in men. Stagnant urine in the bladder can provide a breeding ground for bacteria.
Hormonal Changes
Impact of Menstruation and Menopause:
- Menstruation: Menstrual blood can provide a medium for bacterial growth if not properly managed. Additionally, hormonal changes during menstruation can affect the balance of vaginal flora and increase UTI risk.
- Menopause: Postmenopausal women experience decreased estrogen levels, which can lead to changes in the vaginal environment. This can reduce the natural defense mechanisms against bacteria, increasing susceptibility to UTIs.
Pregnancy and UTIs:
- Hormonal Changes: Pregnancy involves significant hormonal changes that can alter the urinary tract’s normal functioning, making it easier for bacteria to proliferate.
- Pressure on the Bladder: The growing uterus exerts pressure on the bladder, which can lead to incomplete bladder emptying and increase the risk of infection.
- Changes in Urinary Flow: Pregnancy can also affect urinary flow and bladder function, contributing to a higher risk of UTIs.
Sexual Activity
How Sex Can Trigger UTIs:
- Introduction of Bacteria: Sexual activity can introduce bacteria into the urethra from the genital or anal areas, increasing the risk of infection. The friction during intercourse can also cause minor irritations that make it easier for bacteria to invade.
- Urinary Tract Irritation: Sexual activity may cause irritation of the urethra, which can make it more susceptible to bacterial infections.
Preventive Measures During Sexual Activity:
- Urinate Before and After: Urinating before and after intercourse can help flush out any bacteria that may have entered the urethra during sex.
- Hydration: Staying well-hydrated promotes regular urination, which helps in flushing out bacteria from the urinary tract.
- Proper Hygiene: Both partners should practice good genital hygiene to reduce the risk of bacterial transfer.
Personal Hygiene Practices
Proper Hygiene vs. Risky Practices:
- Proper Hygiene: Maintaining good personal hygiene, including wiping from front to back, can help prevent the spread of bacteria from the anal region to the urethra. Regular bathing and wearing breathable cotton underwear can also help.
- Risky Practices: Using irritating feminine products such as douches, sprays, or scented tampons can disrupt the natural balance of bacteria and increase the risk of UTIs. Additionally, wearing tight clothing can create a warm, moist environment conducive to bacterial growth.
Influence of Products and Practices:
- Hygiene Products: Products containing fragrances, dyes, or other chemicals can irritate the urethra and alter the natural flora of the genital area. Opting for unscented and hypoallergenic products can help minimize irritation.
- Overuse of Antibiotics: Frequent or inappropriate use of antibiotics for non-bacterial conditions can disrupt the natural balance of microorganisms in the urinary tract and lead to antibiotic-resistant strains of bacteria.
Chronic Medical Conditions
Diabetes and UTIs:
- High Blood Sugar Levels: Elevated blood sugar levels in diabetics can create an environment conducive to bacterial growth. The excess glucose in urine can promote bacterial proliferation.
- Impaired Immune Function: Diabetes can impair the immune system’s ability to fight infections, making individuals more susceptible to UTIs.
Immune System Disorders:
- Compromised Immunity: Conditions such as HIV/AIDS, cancer, or autoimmune diseases can weaken the immune system, making it harder for the body to fight off infections, including UTIs.
- Immunosuppressive Treatments: Treatments that suppress the immune system, such as chemotherapy or long-term use of corticosteroids, can increase susceptibility to infections.
Urinary Tract Abnormalities
Structural Issues and Obstructions:
- Congenital Abnormalities: Structural issues such as a malformed urethra or bladder can lead to incomplete bladder emptying or urine reflux, increasing the risk of UTIs.
- Obstructions: Conditions like kidney stones, bladder stones, or an enlarged prostate can obstruct urine flow, leading to stagnation and increased risk of infection.
Recurrent Stones and Infections:
- Kidney Stones: Stones in the kidneys or bladder can cause irritation and provide a surface for bacterial growth. They can also obstruct urine flow, leading to infections.
- Recurrent UTIs: Frequent UTIs can sometimes be linked to the presence of stones or other structural abnormalities that make it easier for bacteria to persist and cause repeated infections.
By addressing these factors, individuals can better manage and prevent recurrent UTIs. It’s important to consult with healthcare providers for a thorough evaluation and personalized treatment plan tailored to address the specific causes and risk factors contributing to frequent UTIs.
Lifestyle and Behavioral Factors
Lifestyle and behavioral factors play a significant role in the frequency and recurrence of Urinary Tract Infections (UTIs). From hydration and diet to the use of catheters, understanding how these factors influence UTI risk can help in prevention and management. Here’s a comprehensive look at the key lifestyle and behavioral aspects contributing to UTIs.
Fluid Intake and Hydration
Importance of Adequate Water Consumption:
- Dilution of Urine: Drinking sufficient water helps dilute the urine, reducing the concentration of bacteria and making it easier for the body to flush them out.
- Frequent Urination: Adequate hydration promotes regular urination, which is a natural mechanism for eliminating bacteria from the urinary tract. Frequent urination reduces the chance of bacteria accumulating in the bladder.
- Prevention of Stagnation: Proper fluid intake helps prevent urine stagnation, a condition where urine remains in the bladder for too long, providing a fertile environment for bacterial growth.
Effects of Dehydration on UTI Risk:
- Concentrated Urine: Dehydration leads to concentrated urine, which can irritate the urinary tract and make it easier for bacteria to adhere to the bladder wall.
- Reduced Urinary Output: Insufficient fluid intake reduces the frequency of urination, allowing bacteria to linger in the bladder for longer periods.
- Increased Risk of Infection: Dehydration can impair the body’s ability to flush out bacteria effectively, increasing the risk of developing UTIs.
Recommendations for Adequate Hydration:
- Daily Water Intake: Aim to drink at least 8-10 glasses of water per day. Individual needs may vary based on factors such as age, activity level, and climate.
- Hydration Monitoring: Pay attention to urine color; pale yellow indicates adequate hydration, while dark yellow suggests dehydration.
Diet and Nutrition
Impact of Diet on Urinary Health:
- Nutrient Balance: A well-balanced diet supports overall urinary tract health. Nutrients such as vitamins C and D can enhance immune function and help in preventing infections.
- Acidity Levels: Certain foods and beverages can affect the acidity of urine. Acidic urine can sometimes increase the risk of bacterial growth.
Foods and Beverages to Avoid:
- Caffeine and Alcohol: Both caffeine and alcohol can irritate the bladder and increase the frequency of urination, which may exacerbate UTI symptoms.
- Spicy Foods: Spicy foods can irritate the urinary tract and may contribute to discomfort and symptoms associated with UTIs.
- Sugary Foods: High sugar intake can promote bacterial growth, particularly in individuals with diabetes, which increases the risk of UTIs.
Dietary Recommendations:
- Cranberry Products: Some studies suggest that cranberry juice or supplements can help prevent UTIs by preventing bacteria from adhering to the bladder wall. However, more research is needed to confirm its effectiveness.
- High-Fiber Foods: Foods rich in fiber can help maintain regular bowel movements, reducing the risk of bacterial transfer from the anus to the urethra.
Use of Catheters
How Indwelling Catheters Contribute to UTIs:
- Bacterial Introduction: Indwelling catheters can introduce bacteria into the urinary tract, leading to infections. Bacteria can migrate along the catheter and into the bladder.
- Biofilm Formation: Bacteria can form biofilms on the catheter surface, making it difficult to eradicate the infection and increasing the risk of persistent or recurrent UTIs.
- Infection Risk: The presence of a catheter creates a direct pathway for bacteria to enter the bladder, increasing the risk of UTIs, especially if the catheter is not managed properly.
Best Practices for Catheter Care:
- Regular Cleaning: Clean the catheter insertion site and surrounding area regularly with mild soap and water to reduce the risk of infection.
- Proper Maintenance: Ensure that the catheter is correctly positioned and secured to prevent movement and minimize the risk of infection.
- Hydration: Encourage adequate fluid intake to promote regular urination and help flush out bacteria.
- Prompt Replacement: Replace catheters as recommended by healthcare professionals to minimize the risk of infection and ensure proper function.
- Monitoring: Regularly monitor for signs of infection, such as fever, unusual discharge, or changes in urine color or odor. Seek medical attention if any symptoms of infection are observed.
By addressing these lifestyle and behavioral factors—hydration, diet, and catheter care—individuals can significantly reduce their risk of recurrent UTIs and improve their overall urinary health. Adopting these preventive measures and best practices can lead to a better quality of life and fewer instances of uncomfortable and disruptive infections.
Medical Conditions and Treatments
When dealing with recurrent Urinary Tract Infections (UTIs), it is crucial to understand how medical conditions and treatment practices can influence UTI frequency and severity. Key factors include antibiotic resistance, immune system function, and the impact of previous treatments. Here’s an in-depth exploration of these aspects.
Antibiotic Resistance
How Overuse and Misuse of Antibiotics Affect UTIs:
- Development of Resistant Strains: Overuse or inappropriate use of antibiotics can lead to the development of antibiotic-resistant bacteria. These bacteria evolve mechanisms to evade the effects of medications, making infections harder to treat.
- Ineffective Treatment: When bacteria are resistant to common antibiotics, standard treatments may become ineffective. This can result in persistent or recurrent infections that are difficult to manage.
- Increased Healthcare Costs: Resistant infections often require more expensive and potent antibiotics, leading to increased healthcare costs and longer treatment durations.
Strategies to Combat Resistance:
- Appropriate Antibiotic Use: Ensure antibiotics are prescribed based on accurate diagnosis and targeted to the specific bacteria causing the infection. Avoid using antibiotics for viral infections or non-bacterial conditions.
- Complete Prescribed Courses: Always complete the full course of antibiotics as prescribed, even if symptoms improve before finishing the medication. This helps ensure all bacteria are eradicated and reduces the risk of resistance.
- Antibiotic Stewardship: Healthcare providers should practice antibiotic stewardship, which involves selecting the appropriate antibiotic at the right dose and duration, and avoiding unnecessary prescriptions.
- Patient Education: Educate patients on the importance of proper antibiotic use and the risks of misuse. Promote understanding of how improper use contributes to resistance.
Immune System Function
How a Compromised Immune System Affects UTI Risk:
- Reduced Ability to Combat Infections: A weakened immune system, whether due to chronic diseases, medications, or other factors, diminishes the body’s ability to effectively fight off infections, including UTIs.
- Increased Susceptibility: Individuals with compromised immune systems are more susceptible to infections, including UTIs, as their bodies are less able to mount a robust defense against invading bacteria.
- Prolonged Infections: Infections may become more severe and last longer in individuals with weakened immune systems, leading to more frequent or recurrent UTIs.
Factors Affecting Immune System Function:
- Chronic Diseases: Conditions such as diabetes, HIV/AIDS, and cancer can impair immune function, increasing the risk of UTIs.
- Medications: Immunosuppressive drugs, including corticosteroids and chemotherapy agents, can weaken the immune system and make individuals more vulnerable to infections.
- Nutritional Status: Poor nutrition can negatively impact immune function. Adequate intake of essential nutrients is crucial for maintaining a healthy immune system.
Previous UTI Treatments
Incomplete Courses and Their Effects:
- Risk of Recurrence: Not completing a prescribed course of antibiotics can lead to incomplete eradication of the bacteria, resulting in a recurrence of the infection.
- Development of Resistance: Incomplete courses can contribute to the development of antibiotic-resistant bacteria, complicating future treatments and increasing the risk of persistent infections.
- Persistent Symptoms: Partial treatment may alleviate symptoms temporarily but leave underlying bacteria that can cause recurrent infections.
Impact of Repeated Treatments:
- Increased Risk of Resistance: Frequent use of antibiotics for recurrent UTIs can increase the likelihood of developing antibiotic-resistant strains. This makes subsequent infections harder to treat and may require the use of more potent and less commonly used antibiotics.
- Impact on Microbiota: Repeated antibiotic use can disrupt the natural balance of microorganisms in the urinary tract and surrounding areas. This imbalance can increase susceptibility to infections and lead to further complications.
- Treatment Complications: Repeated treatments can sometimes lead to adverse effects, including allergic reactions, gastrointestinal disturbances, and other side effects associated with antibiotics.
Best Practices for Managing Previous Treatments:
- Follow-Up Care: Regular follow-up with a healthcare provider is essential for monitoring UTI recurrence and ensuring appropriate treatment. This includes assessing the effectiveness of previous treatments and making necessary adjustments.
- Culture and Sensitivity Testing: Conducting urine culture and sensitivity tests before starting treatment can help identify the specific bacteria causing the infection and determine the most effective antibiotic.
- Preventive Measures: In addition to treating current infections, consider preventive strategies such as lifestyle modifications, prophylactic antibiotics (when appropriate), and management of underlying conditions to reduce the risk of future UTIs.
Understanding the influence of antibiotic resistance, immune system function, and the impact of previous treatments on recurrent UTIs is essential for effective management and prevention. By addressing these factors, individuals and healthcare providers can work together to improve treatment outcomes, reduce recurrence, and maintain overall urinary health.
Diagnostic Approaches
Accurate diagnosis is crucial for managing recurrent Urinary Tract Infections (UTIs) effectively. Identifying the underlying causes of frequent UTIs, utilizing appropriate diagnostic tests, and understanding the role of urine cultures and sensitivity testing are essential steps in developing an effective treatment and prevention plan. Here’s a comprehensive look at the diagnostic approaches for recurrent UTIs.
Identifying the Underlying Causes
Understanding Underlying Causes:
- Anatomical Abnormalities: Structural issues such as bladder diverticula, urinary reflux, or congenital abnormalities can predispose individuals to recurrent UTIs. Identifying these abnormalities helps in targeting specific treatments or surgical interventions.
- Chronic Conditions: Chronic medical conditions like diabetes, immune system disorders, or kidney stones can contribute to frequent UTIs. Diagnosing these conditions allows for comprehensive management that addresses both the UTI and its underlying cause.
- Behavioral Factors: Factors such as inadequate fluid intake, poor hygiene practices, and frequent use of irritants can also contribute to recurrent UTIs. Identifying these behaviors can lead to lifestyle modifications that reduce infection risk.
Comprehensive Evaluation:
- Patient History: A detailed medical history, including previous UTI episodes, treatment responses, and any associated symptoms, is crucial for identifying patterns and potential underlying causes.
- Physical Examination: A thorough physical examination can reveal signs of anatomical abnormalities or complications related to recurrent UTIs.
Diagnostic Tests and Procedures
Common Diagnostic Tests:
- Urinalysis: A basic test that examines the appearance, concentration, and content of urine. It helps in detecting signs of infection, such as the presence of white blood cells, red blood cells, or nitrites.
- Urine Culture: A test that grows bacteria from a urine sample to identify the specific type of bacteria causing the infection. This test is crucial for diagnosing bacterial infections and determining the most effective antibiotic treatment.
- Imaging Studies: Procedures such as ultrasound, CT scans, or MRIs can visualize the urinary tract and identify structural abnormalities, stones, or other issues that may contribute to recurrent infections.
- Cystoscopy: A procedure that involves inserting a thin tube with a camera into the bladder through the urethra. It allows direct visualization of the bladder and urethra to identify abnormalities or sources of infection.
Specialized Tests:
- Urodynamic Studies: Tests that assess how well the bladder and urethra are functioning. These studies can help identify issues with bladder emptying or pressure that may contribute to UTIs.
- Voiding Cystourethrogram (VCUG): An imaging test that involves filling the bladder with contrast dye and taking X-rays to observe how urine flows through the bladder and urethra. It helps identify reflux or other functional issues.
Importance of Accurate Diagnosis
Tailored Treatment:
- Effective Antibiotic Use: Accurate diagnosis ensures that the appropriate antibiotic is selected based on the specific bacteria causing the infection. This helps in effective treatment and reduces the risk of antibiotic resistance.
- Addressing Underlying Causes: Identifying the underlying causes of recurrent UTIs allows for targeted treatments that address both the infection and its root causes, improving long-term outcomes.
Prevention of Complications:
- Avoiding Misdiagnosis: An accurate diagnosis helps prevent unnecessary treatments or incorrect management, which could lead to complications such as persistent infections or damage to the urinary tract.
- Early Intervention: Proper diagnosis allows for early intervention in cases of chronic conditions or structural abnormalities, preventing the progression of disease and reducing the risk of severe complications.
Role of Urine Cultures and Sensitivity Testing
Urine Cultures:
- Identifying Pathogens: Urine cultures identify the specific bacteria causing the infection. This is crucial for diagnosing the type of infection and selecting the most effective antibiotic.
- Determining Resistance: Cultures can reveal whether the bacteria are resistant to commonly used antibiotics, guiding the choice of medication and helping to avoid ineffective treatments.
Sensitivity Testing:
- Selecting Effective Antibiotics: Sensitivity testing determines which antibiotics are effective against the bacteria identified in the urine culture. This ensures that the prescribed antibiotic will successfully eliminate the infection.
- Personalized Treatment: By understanding the bacteria’s susceptibility to various antibiotics, sensitivity testing allows for a more personalized and effective treatment approach, reducing the risk of recurrence and complications.
How Testing Helps Identify Persistent Issues:
- Detecting Resistant Strains: Sensitivity testing can identify antibiotic-resistant strains of bacteria, which may require alternative treatments or strategies to manage recurrent infections.
- Identifying Biofilms: In cases of chronic infections, testing can sometimes reveal biofilms—clusters of bacteria that adhere to surfaces in the urinary tract and are difficult to eradicate. This may necessitate specialized treatment approaches.
- Assessing Treatment Efficacy: Regular testing during and after treatment helps assess whether the infection is resolving and guides adjustments to the treatment plan if needed.
In summary, effective management of recurrent UTIs relies on a comprehensive diagnostic approach that includes identifying underlying causes, utilizing appropriate tests and procedures, and understanding the role of urine cultures and sensitivity testing. Accurate diagnosis is essential for tailored treatment, prevention of complications, and overall improvement in urinary health.
Prevention and Management Strategies
Managing and preventing recurrent Urinary Tract Infections (UTIs) involves a combination of lifestyle changes, proper hygiene, and targeted medical interventions. Effective strategies can help reduce the frequency of UTIs and improve overall urinary health. Here’s a comprehensive guide to prevention and management strategies for recurrent UTIs.
Preventive Measures
Lifestyle Changes to Reduce UTI Risk:
- Increase Fluid Intake: Drinking plenty of water helps flush out bacteria from the urinary tract and dilutes urine, reducing the risk of infection. Aim for at least 8-10 glasses of water per day.
- Regular Urination: Avoid holding urine for long periods. Regular urination helps to expel bacteria before they can establish an infection.
- Healthy Diet: Incorporate a balanced diet rich in vitamins and minerals that support urinary health. Some studies suggest that cranberry products may help prevent UTIs by preventing bacteria from adhering to the bladder wall, although more research is needed.
- Manage Diabetes: If you have diabetes, keep blood sugar levels well-controlled to reduce the risk of UTIs. High blood sugar can provide a fertile environment for bacterial growth.
- Avoid Irritants: Reduce the consumption of bladder irritants such as caffeine, alcohol, and spicy foods. These can exacerbate UTI symptoms and increase susceptibility.
Importance of Proper Hygiene and Hydration:
- Good Personal Hygiene: Maintain proper hygiene by wiping from front to back after using the toilet. This reduces the risk of transferring bacteria from the anal area to the urethra.
- Use Mild Products: Choose unscented, mild soap for genital hygiene. Avoid douches, sprays, and other products that can disrupt the natural balance of bacteria.
- Hydration Practices: Regular hydration is crucial for urinary health. Ensure that you drink water throughout the day, especially before and after activities that may increase UTI risk.
Medical Interventions
Prophylactic Antibiotics and Their Use:
- When Prophylaxis is Recommended: Prophylactic antibiotics may be prescribed for individuals with frequent UTIs, especially if the infections are recurrent despite lifestyle modifications and other preventive measures. This approach can be considered in cases of severe or persistent UTIs.
- Types of Prophylactic Antibiotics: Low-dose antibiotics may be taken daily or after certain activities (such as sexual intercourse) to prevent the onset of infection. The choice of antibiotic should be based on urine culture results and susceptibility testing.
- Risks and Benefits: While prophylactic antibiotics can reduce the frequency of UTIs, they may also contribute to antibiotic resistance and other side effects. It is essential to weigh these risks against the benefits and to follow medical guidance carefully.
Treatment Options for Underlying Conditions:
- Addressing Anatomical Abnormalities: Structural issues such as bladder diverticula, urethral abnormalities, or obstructions may require surgical intervention or other treatments to prevent recurrent UTIs.
- Managing Chronic Diseases: For conditions like diabetes or immune disorders, effective management of the underlying disease is crucial. This may involve medication adjustments, lifestyle changes, and regular monitoring to reduce UTI risk.
- Treating Urinary Tract Abnormalities: Conditions such as urinary reflux or bladder stones may need specific treatments or surgical interventions to correct the issue and prevent recurrent infections.
Regular Monitoring and Follow-Up:
- Routine Check-Ups: Regular visits to a healthcare provider can help monitor UTI recurrence and adjust treatment plans as necessary. Follow-up care is important for managing chronic conditions and preventing complications.
- Monitoring Symptoms: Keep track of any UTI symptoms or changes in urinary habits and report them to your healthcare provider. Early intervention can help prevent complications and manage infections more effectively.
Behavioral and Lifestyle Modifications:
- Sexual Activity: If sexual activity is a trigger for UTIs, consider preventive measures such as urinating before and after intercourse, using lubrication, and maintaining good genital hygiene. Discuss alternative methods or strategies with your healthcare provider if needed.
- Hygiene Products: Use hypoallergenic and non-irritating personal hygiene products to minimize the risk of disrupting the natural balance of bacteria in the genital area.
In summary, preventing and managing recurrent UTIs requires a multifaceted approach that includes lifestyle modifications, proper hygiene, and targeted medical interventions. By adopting preventive measures, addressing underlying conditions, and utilizing medical treatments appropriately, individuals can significantly reduce their risk of recurrent infections and improve their overall urinary health. Regular communication with healthcare providers and adherence to prescribed treatments are essential components of effective UTI management.
When to Seek Medical Help
Knowing when to seek medical help for a Urinary Tract Infection (UTI) is crucial for effective management and prevention of complications. Recognizing signs of complications, understanding when a UTI might be severe or recurrent, and knowing when to consult a specialist can significantly impact the outcome of treatment. Here’s a detailed guide on these aspects.
Signs of Complications
Recognizing Severe or Complicated UTIs:
- Persistent Symptoms: If symptoms persist despite completing a prescribed course of antibiotics, this may indicate a more severe or complicated UTI that requires further evaluation.
- Severe Pain: Intense or worsening pain in the lower abdomen, pelvis, or back, especially if accompanied by fever, may suggest a kidney infection (pyelonephritis) or other serious complications.
- High Fever: A high fever, particularly if it exceeds 101°F (38.3°C), can be a sign of a more severe infection or systemic involvement. It may indicate that the infection has spread beyond the urinary tract.
- Nausea and Vomiting: These symptoms, along with fever and pain, can be signs of a kidney infection or other serious complications. Vomiting can also lead to dehydration, exacerbating the infection.
- Blood in Urine: Hematuria (blood in urine) can be a sign of a complicated UTI or another underlying issue. If blood is visible in the urine, it’s essential to seek medical evaluation promptly.
- Signs of Systemic Infection: Symptoms such as chills, shaking, rapid heartbeat, or confusion may indicate that the infection has spread to the bloodstream (sepsis) and requires immediate medical attention.
Recognizing Recurrent UTIs:
- Frequent Infections: If UTIs occur more than twice in six months or more than three times in a year, it’s important to consult a healthcare provider to evaluate potential underlying causes and develop a comprehensive management plan.
- Change in Symptoms: A change in the pattern of symptoms or new symptoms, such as pain during urination or unusual discharge, should prompt a medical consultation to assess for possible complications or resistance.
Specialist Referrals
When to Consult a Urologist or Specialist:
- Recurrent or Chronic UTIs: Frequent or persistent UTIs that do not respond to standard treatments may require a urologist's evaluation. A urologist specializes in urinary tract issues and can perform advanced diagnostic tests and recommend specialized treatments.
- Anatomical Abnormalities: If imaging or diagnostic tests reveal structural abnormalities in the urinary tract, such as bladder diverticula, urinary reflux, or obstructions, a urologist can provide targeted treatments or surgical interventions.
- Complex Medical Conditions: Individuals with complex medical conditions like diabetes, immunosuppressive disorders, or chronic kidney disease may benefit from a specialist's care to manage both the UTI and the underlying condition effectively.
- Resistance to Antibiotics: If recurrent UTIs are caused by antibiotic-resistant bacteria, a urologist or infectious disease specialist may be needed to develop an alternative treatment plan and address resistance issues.
- Complicated UTIs: In cases of severe UTIs, such as those involving kidney infections or systemic infections, specialist care may be necessary for comprehensive management and to prevent complications.
Referral Process:
- Primary Care Physician: Start by consulting with your primary care physician, who can provide initial treatment and referrals to specialists if needed. They can also help coordinate care and ensure that all aspects of your health are addressed.
- Specialist Consultation: Based on your symptoms and medical history, your primary care physician may refer you to a urologist or infectious disease specialist. The specialist will conduct a thorough evaluation, including diagnostic tests and a review of your medical history, to provide tailored treatment recommendations.
Preparing for Specialist Visits:
- Document Symptoms: Keep a record of your symptoms, including their frequency, duration, and any changes in pattern. This information will help the specialist understand your condition better.
- Medical History: Prepare a summary of your medical history, including previous UTIs, chronic conditions, and any medications or treatments you have undergone. This background will assist the specialist in diagnosing and managing your condition.
- Questions and Concerns: Prepare a list of questions and concerns to discuss with the specialist. This can help ensure that all your issues are addressed during the consultation.
In summary, knowing when to seek medical help for UTIs involves recognizing signs of complications, understanding the importance of addressing recurrent infections, and knowing when to consult a specialist. Early intervention and appropriate specialist care can prevent complications, address underlying issues, and improve the overall management of UTIs. Regular communication with healthcare providers and timely referrals to specialists are key components of effective UTI management and prevention.
Shri Chyawan’s Ayurvedic Solution
Urinary Infection: Urinary Infection causes problems in the urinary system such as kidney, and bladder infections. Most of the infections take place in the lower urinary tract. If, these urinary infections whether in men or women are not treated in time, then they might result in kidney damage.
Symptoms of Urinary infection: This mostly depends on which part of the urinary tract has been infected, symptoms of these include:
- Burning/inflammation sensation while urinating
- Frequent urination
- Cloudy urine
- Color change in urine
Shri Chyawan Ayurveda's Urinating Care Kit includes the following:
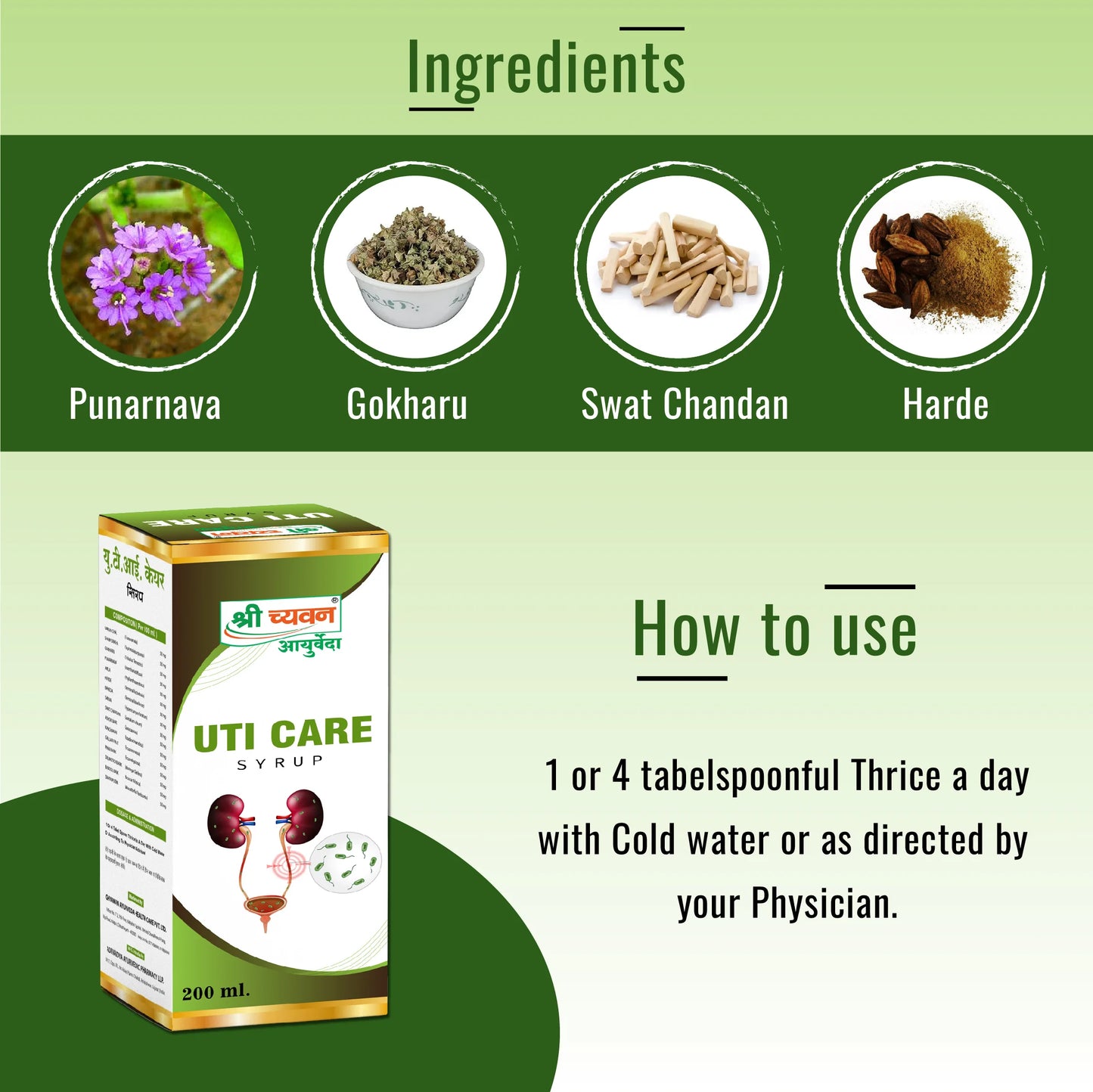
1. Uti Care Syrup: One of the effective ayurvedic syrup for urine infection, useful in curing Urine Infections and Urine blockages. It also acts as a detoxifier for your body and cleanses your system.
Ingredients: It consists of mainly Varun Chal, Sharpunkha, Gokharu, Punarnava, Amle, Harde, Baheda, Sariva, Swat Chandan, Ashok Bark, Kanchanar, Gullar Fruit, Pipar Bark, Drumstick Bark, Babbol Bark, Dhatkipuspa.
How to use: Consume 1 teaspoon thrice a day with cold water or as directed by the physician.
2. Chandraprabha Vati: Chandraprabha Vati helps to reduce the level of uric acid, which aids in keeping urinary infections away.
Ingredients: It consists Swarn Bhasm, Vai Vidang, Chitrak Bark, Daruharidra, Devdaru, Camphor, Pipalmool, Nagarmotha, Pippal, Kali Mirch, Yavkshar, Vach, Dhania, Chavya, Gajpipal, Sounth, Sendha Namak, Nishoth, Dantimool, Tejpatra, Chhoti elaichi.
How To Use: Consume 1 tablet at night before going to bed. consulting a healthcare professional before use.
Conclusion
Managing and preventing Urinary Tract Infections (UTIs) effectively requires a comprehensive understanding of their causes, diagnostic approaches, and treatment options. In this blog, we have explored the critical aspects of UTIs, including their causes, diagnostic methods, and management strategies. Here’s a recap of the key points discussed and an encouragement for proactive management.
Recap of Key Points
- Definition and Types: UTIs occur when bacteria enter the urinary tract and cause infection. They can affect various parts of the urinary system, including the bladder (cystitis), kidneys (pyelonephritis), and urethra (urethritis).
- Common Causes: Factors such as anatomical abnormalities, hormonal changes, sexual activity, and personal hygiene practices contribute to the development of UTIs.
- Identifying Underlying Causes: Accurate diagnosis involves understanding potential underlying causes such as anatomical abnormalities or chronic conditions that may predispose individuals to recurrent infections.
- Diagnostic Tests: Essential tests include urinalysis, urine cultures, imaging studies, and, in some cases, specialized procedures like cystoscopy. These tests help identify the causative bacteria, assess resistance, and detect any structural issues.
- Preventive Measures: Lifestyle changes, such as increasing fluid intake, maintaining proper hygiene, and avoiding irritants, are crucial for reducing UTI risk.
- Medical Interventions: Prophylactic antibiotics may be prescribed for individuals with frequent UTIs, and treating underlying conditions is vital for long-term management. Regular follow-up with healthcare providers ensures effective treatment and prevention of complications.
- Signs of Complications: Persistent symptoms, severe pain, high fever, nausea, vomiting, or blood in the urine warrant immediate medical attention. Recognizing these signs helps prevent serious complications.
- Specialist Referrals: Frequent or severe UTIs, anatomical abnormalities, complex medical conditions, and antibiotic resistance may require consultation with a urologist or infectious disease specialist.
Encouragement for Proactive Management
Managing UTIs effectively involves a proactive and comprehensive approach. Here’s how you can take charge of your urinary health:
- Stay Informed: Educate yourself about UTIs, their causes, and the best practices for prevention and treatment. Knowledge empowers you to make informed decisions about your health.
- Adopt Preventive Measures: Implement lifestyle changes that reduce your risk of UTIs. Simple practices like staying hydrated, practicing good personal hygiene, and avoiding irritants can make a significant difference.
- Follow Medical Advice: Adhere to prescribed treatments and attend follow-up appointments. Complete antibiotic courses as directed, and communicate any concerns or changes in symptoms to your healthcare provider.
- Seek Early Intervention: Don’t wait for symptoms to worsen. Seek medical help promptly if you experience signs of a UTI or complications. Early intervention can prevent the progression of the infection and reduce the risk of long-term issues.
- Engage in Regular Monitoring: For individuals with recurrent UTIs or chronic conditions, regular monitoring and preventive care are essential. Work closely with your healthcare provider to manage your condition effectively.
In conclusion, a proactive approach to UTI management not only helps in preventing recurrent infections but also enhances overall urinary health. By staying informed, adopting preventive measures, following medical advice, and seeking timely medical help, you can effectively manage UTIs and maintain a better quality of life.
FAQs: Common Questions and Answers About Frequent UTIs
Frequent Urinary Tract Infections (UTIs) can be concerning and confusing, leading to many common questions. This section addresses some of the most frequently asked questions about recurrent UTIs, offering clear and informative answers to help you understand and manage these infections more effectively.
1. What Causes Frequent UTIs?
Answer: Frequent UTIs can be caused by various factors including anatomical abnormalities (such as urinary reflux or bladder diverticula), hormonal changes (such as those during menopause), chronic conditions (like diabetes), and behavioral factors (such as infrequent urination or poor personal hygiene). In some cases, underlying medical conditions or repeated use of antibiotics can also contribute to recurrent infections.
2. How Can I Prevent Recurrent UTIs?
Answer: Preventive measures include:
- Increasing Fluid Intake: Drink plenty of water to help flush out bacteria from the urinary tract.
- Maintaining Proper Hygiene: Wipe from front to back and use mild, unscented products for genital hygiene.
- Urinate Regularly: Avoid holding urine for long periods.
- Post-Sexual Hygiene: Urinate after sexual intercourse and consider using a water-based lubricant to reduce irritation.
- Dietary Considerations: Some studies suggest that cranberry products may help prevent UTIs, though more research is needed.
3. When Should I See a Doctor for a UTI?
Answer: You should consult a healthcare provider if:
- Symptoms Persist: Symptoms continue despite completing a course of antibiotics.
- Severe Symptoms: You experience severe pain, high fever, nausea, vomiting, or blood in the urine.
- Frequent Recurrence: You have recurrent UTIs (more than twice in six months or three times a year).
- New Symptoms: You notice a change in symptoms or new symptoms.
4. What Tests Are Used to Diagnose UTIs?
Answer: Diagnostic tests for UTIs typically include:
- Urinalysis: To check for signs of infection like white blood cells, red blood cells, and nitrites.
- Urine Culture: To identify the specific bacteria causing the infection and determine antibiotic sensitivity.
- Imaging Studies: Such as ultrasound or CT scans, to detect structural abnormalities or complications.
- Cystoscopy: For direct visualization of the bladder and urethra if needed.
5. How Are Recurrent UTIs Treated?
Answer: Treatment for recurrent UTIs involves:
- Antibiotics: Tailored to the specific bacteria identified in urine cultures. Prophylactic antibiotics may be considered for frequent infections.
- Addressing Underlying Causes: Treating any underlying conditions or anatomical abnormalities.
- Lifestyle and Behavioral Modifications: Implementing preventive measures to reduce risk.
6. What Are Prophylactic Antibiotics and When Are They Used?
Answer: Prophylactic antibiotics are low-dose antibiotics taken regularly or after specific activities (like sexual intercourse) to prevent the recurrence of UTIs. They are used in individuals with frequent or severe UTIs and are prescribed based on the patient’s history and risk factors.
7. Can UTIs Be Managed Without Antibiotics?
Answer: While antibiotics are often necessary to treat active infections, some preventive measures and lifestyle changes can help reduce the frequency of UTIs. These include staying hydrated, practicing good hygiene, and managing underlying conditions. However, if a UTI does occur, antibiotics are typically required for effective treatment.
8. Are There Any Risks Associated with Repeated Antibiotic Use?
Answer: Yes, repeated use of antibiotics can lead to:
- Antibiotic Resistance: Bacteria may become resistant to commonly used antibiotics, making future infections harder to treat.
- Disruption of Normal Flora: Repeated antibiotics can disrupt the natural balance of microorganisms in the urinary tract and surrounding areas.
9. How Can I Manage UTIs if I Have a Chronic Condition Like Diabetes?
Answer: For individuals with chronic conditions such as diabetes, managing blood sugar levels is crucial to reducing UTI risk. Regular monitoring, effective treatment of infections, and maintaining good overall health can help prevent complications and recurrent infections.
Free Consultation with our Expert Doctor- 📞📞 95162 64444